Fungal nail infection – Causes, signs, and management

Onychomycosis is a condition that affects fingernails or toenails. Also known as nail fungal infection or fungal nail infection, the condition can cause pain, discoloration, and swelling. While fungi naturally may exist in the surroundings or inhabit the human body, sometimes, an overgrowth of fungi causes infections. The infection can spread within the body and from one person to another if left unchecked. So, it is important to seek timely treatment upon noticing common signs.
Causes and risk factors
The following factors may contribute to these infections:
Humid or moist environments: Fungi thrive in warm and moist environments, making public swimming pools, locker rooms, and showers common breeding grounds.
Inadequate hygiene: Poor foot hygiene, including not drying feet properly after washing, can create a conducive environment for fungal growth.
Nail trauma: Injuries or nail trauma can damage the nail, making it more susceptible to infection.
Profuse sweating: Those who are prone to heavy perspiration may be at a higher risk of developing fungal infections in their nails.
Weakened immune system: Those with compromised immune systems are at a higher risk of developing nail fungal infections.
Age and genetics: Aging and genetic predisposition can make some more prone to nail fungal infections.
Other health conditions: Diabetes, athlete’s foot, psoriasis, HIV, and cancer can make one more vulnerable to onychomycosis.
Certain lifestyle choices: Wearing artificial nails, plastic gloves, socks, and tight shoes that prevent ventilation for extended periods of time can make one more susceptible to the infection. Similarly, undergoing manicure and pedicure treatments with unsterilized tools is also a risk factor.
Symptoms
Recognizing the symptoms of a nail fungal infection is crucial for seeking early intervention. Common signs include:
Thickened nails: Infected nails can become thicker and may change in shape.
Discoloration: Nails may turn yellow, brown, or white and can become dark or cloudy when dealing with fungal infections
Brittle or crumbly nails: Infected nails tend to become brittle. They may also easily separate from the nail bed.
Distorted nail shape: The shape of the nail may become distorted or irregular due to the infection.
Pain and discomfort: In severe cases, fungal nail infections can cause pain and discomfort, particularly if left untreated.
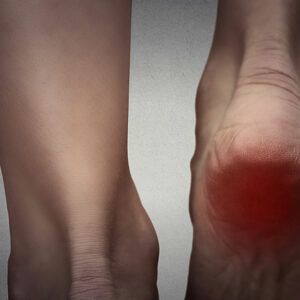
Bleeding or swelling: Inflammation or bleeding around the nails may be observed when dealing with a fungal infection. Such signs should prompt one to seek immediate medical intervention.
Foul odor: One may notice an unusual smell around their nails, which can indicate a fungal growth.
Management options
Common treatment options for nail fungal infection include:
– Certain antifungal creams, gels, and nail coatings can work for mild cases of infections. However, one should follow the instructions carefully and consult a health professional for optimal results. Further, these products may take several months to show results, so it is important to be patient.
– Laser treatments have emerged as a non-invasive option for treating nail fungal infections. The procedure targets the fungi while sparing the healthy nail tissue.
– Surgery can remove the affected nail in cases where the infection does not respond to other treatments. This option may be necessary to allow a new, healthy nail to grow.
– Natural solutions like tea tree oil or vinegar soaks could be considered. While these methods may offer some relief, their effectiveness varies, and they cannot replace treatment.